The Guanabenz Trial for VWM is underway! Click here for more information, and check out the Vanishing White Matter Consortium clinical trial page!
Read an update regarding the future of clinical trials for VWM.
“Guanabenz is an alpha2-adrenergic antihypertensive drug with proven safety in adults. Evidence also supports safe use in children aged 12 years and older. Recently, guanabenz has been shown to impact the ISR and currently is the only registered drug with a known effect on the ISR. The ameliorating effect of guanabenz on VWM has been substantiated in a VWM mouse model representative for the human disease.”
– Netherlands Trial Register, Guanabenz Trial Summary
The VWM Registery is officially open! The Center for Childhood White Matter Disorders at the VU University Medical Center (VUmc) in Amsterdam, The Netherlands, has developed an online Registry for patients with Vanishing White Matter (VWM). The aim of the Registry is to collect as much insight in the disease course as possible, regarding both clinical features and MRI. This database will play an important role in developing treatment strategies and making decisions regarding therapeutic trials. Information is needed on as many patients as possible, even if patients are no longer alive. Register via: registerVWM@vumc.nl
What is Vanishing White Matter Disease?
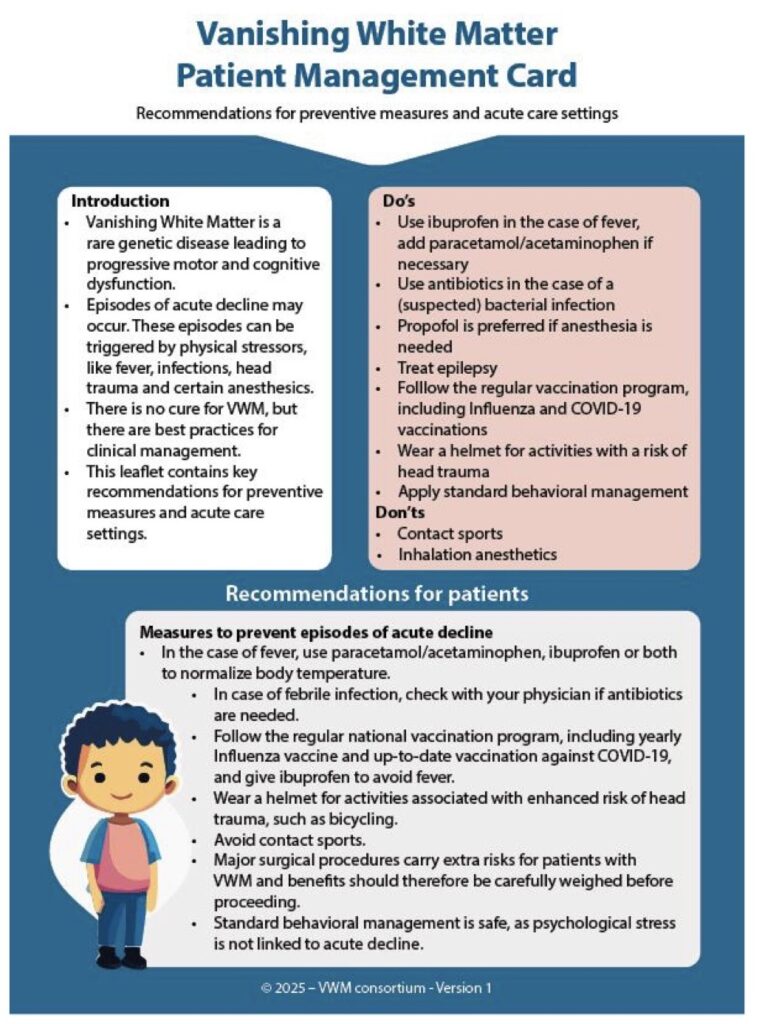
Vanishing White Matter Disease (VWM) is a genetic disorder that affects the nervous system and causes neurologic symptoms. Although initially recognized as a disease of young children, it is now known that the disease has a highly variable course with a wide range in severity. A striking feature of VWM is that in addition to a generally slow progression of symptoms, patients may show episodes of rapid neurological deterioration in response to certain stressors, such as infection or minor head trauma. The patient may partially recover following these episodes, but in severe cases the episode may even lead to coma and death.
What are the symptoms of VWM?
The disease characteristics are highly variable. The course varies from antenatal onset with death in the first months of life up to first presentation in later adulthood with only mild neurological problems. Age of onset of disease features is an important predictor for disease course. The largest group of patients presents in early childhood (at the age of 2-3 years). Generally, a child with VWM will appear relatively normal at birth, though he/she may have slightly delayed psychomotor development. At a certain point, loss of motor function is noticed, which can be triggered by a specific stressor, such as an infection with fever or head trauma. From that moment onwards there is a chronic neurological deterioration, often as well as episodic deterioration caused by stressors. Patients with onset in later childhood or even adulthood (~15% of cases have an onset after the age of 18 years) may present with less typical features such as memory problems or behavioral changes. These patients have a less severe disease course.
We have listed some possible symptoms below as well as definitions as necessary:
- Chronic neurological deterioration, mainly with loss of motor skills
- Febrile episodes (episodes of fever) can be associated with worsening of symptoms, drowsiness or coma.
- Cerebellar ataxia: loss of muscle coordination and balance.
- Spasticity: This means that the child tends to suffer spasms or involuntary contractions of
Muscles are abnormally stiff and movement is restricted. - Seizures: well controlled with medication in most patients, but some patients have severe
epilepsy not responding to medication - Optic atrophy (variably present): an abnormality of nerves of the eyes.
- Ovarian dysgenesis in female patients: defective development of the ovaries, which can result in lack of menstrual periods, fertility problems and early menopause.
- Mental decline may be present, though generally less severe than the motor dysfunction
- Lethargy: Abnormal drowsiness and indifference to environmental stimuli
- Coma
- Death: may occur after a variable period, depending on disease severity, ranging from a few months in patients who present in the first year of life, a few years in patients presenting in early childhood and a few decades in patients who present in later childhood. Patients who present later in life may have a normal life expectancy.
The motor difficulties in VWM are progressive, and the progression is often partially stepwise in association with fever or injuries. After an episode of deterioration there may be partial improvement, but some episodes result in permanent loss of neurological function and sometimes coma or death.
What causes VWM?
VWM is caused by mutations in one of the five genes EIF2B1, EIF2B2, EIF2B3, EIF2B4 and EIF2B5 that encode the five subunits of a protein called eukaryotic initiation factor 2B (eIF2B). This protein is necessary for the production of all other proteins in the body and for the regulating the rate of protein production, especially the decrease in protein synthesis during stress conditions, such as fever and infection. It is so important that no one can live when any of these genes are completely non-functional or absent. VWM is caused by small changes in these genes that reduce the function of eIF2B, and specific cells in the brain are particularly vulnerable to this loss of function. The reduction in function becomes a particular problem during episodes of fever, infection, or head trauma, and deterioration accelerates following such episodes (see What are the symptoms of VWM).
How is VWM inherited?
VWM is inherited in an autosomal recessive manner. This means that both parents carry one copy of a mutated eIF2B gene and pass it along to their child, who then has two copies of the mutated gene and develops the disease. Parents who have one copy of the mutated gene and a second normal gene are genetic carriers of the abnormal gene, but do not have symptoms. For each pregnancy, carrier parents have a 25% chance of having a child affected by the disorder
How is VWM diagnosed?
VWM is diagnosed on the basis of the clinical symptoms in combination with the results of a Magnetic Resonance Imaging (MRI) scan of the brain, which shows a distinctive pattern of abnormalities of the white matter of the brain. Subsequently, DNA analysis of the eIF2B genes can identify the genetic defect.
What is the treatment for VWM?
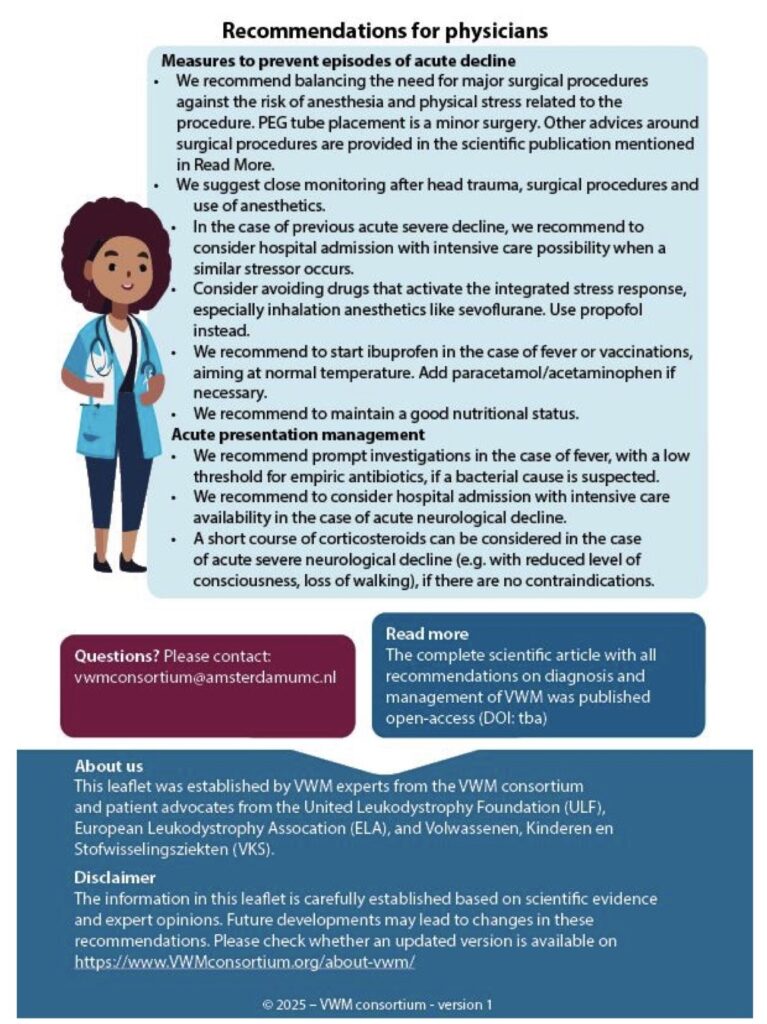
There is currently no cure for VWM; treatment is directed at the symptoms as they arise. It is extremely important to prevent episodes of deterioration, especially in young children, by preventing and treating infections and fever when possible through the use of vaccinations, antibiotics for minor infections and antipyretics for fever. Prevention of mild head trauma is warranted at all ages. For children, wearing a helmet outside helps minimize the effects of head trauma.
How is scientific research on VWM progressing towards improved treatment or diagnosis?
The identification of the genetic basis of VWM was a great step forward. First of all, it allows genetic testing for the disease. If you know that the disease runs in your family, you can talk to a genetic counselor about the option of prenatal testing, as well as testing of family members so that they can find out if they are carriers of the disease (see our fact sheet on genetic inheritance for more information about this). Secondly, it allows further research on the underlying disease mechanism, which is fundamental for the eventual development of treatment. The current research includes studies on the understanding of the effect of mutations in eIF2B and on the development of stem cell therapy, gene therapy and medicines that reduce the neurological deterioration.
Are there other names for VWM?
Other clinical names for VWM include:
- Childhood Ataxia with diffuse CNS Hypomyelination (CACH)
- Vanishing White Matter Leukodystrophy
- Cree Leukoencephalopathy
- Leukodystrophy with Ovarian Failure
- Ovarioleukodystrophy
- eIF2B-related disorders
Read “Consensus-Based Expert Recommendations for Diagnosis and Clinical Management of Vanishing White Matter“ full article here: Neurology Journal – van Voorst R.J. et al., 2025