by The Montreal Children’s Hospital Foundation
Dr. Geneviève Bernard is a world-renowned expert on genetically determined white matter disorders, called leukodystrophies.
Patients are referred to her clinic from all over the world. She brings much comfort to families everywhere who are suffering from these diseases for which the vast majority currently have no known cure.
Dr. Bernard started her career as an independent investigator and pediatric neurologist in 2011 at the Montreal Children’s Hospital of the McGill University Health Center (MUHC) and the Research Institute of the MUHC. She is currently an Associate Professor at McGill University, in the Departments of Neurology and Neurosurgery, Pediatrics and an associate member of the Department of Human Genetics.
She is also the 2019 recipient of the Prix d’excellence – Specialist of the Year Award from the Royal College of Physicians and Surgeons of Canada.
At the beginning of April, we checked in with Dr. Bernard about how things were going in this new reality.
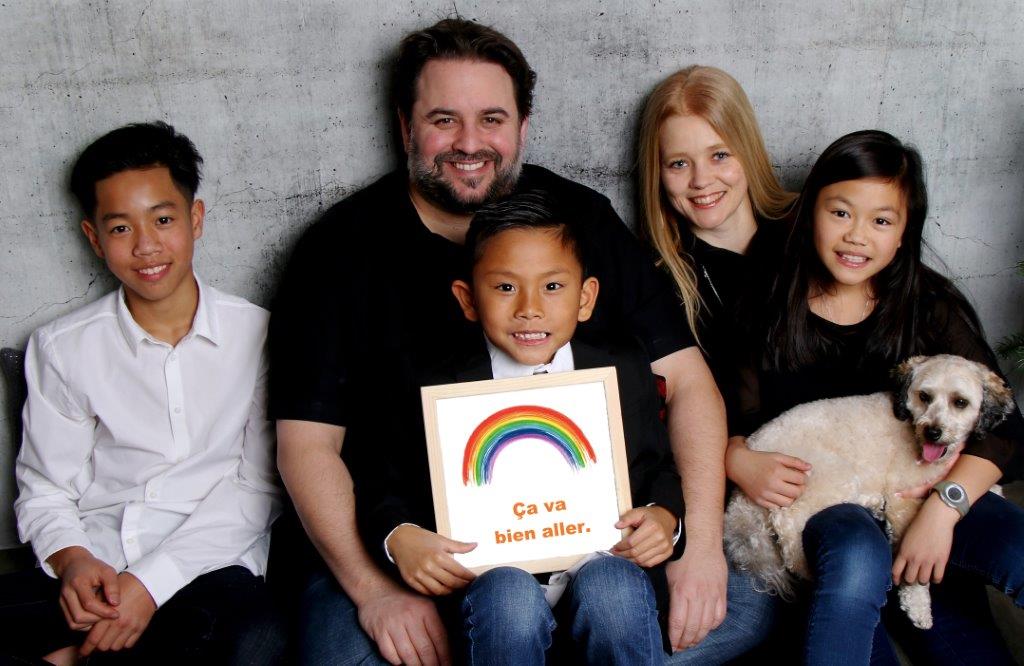
How are you and your family coping?
GB: I’m OK. My husband and I quickly set ourselves up to work from home, which was reassuring for everyone. My three kids feel that this is a different situation and are getting along quite well actually, most of the time!
Dr. Bernard follows more than 100 patients per year, and since they are all complex and vulnerable, she had to adjust rapidly to new guidelines in caring for them.
What is happening with your clinical practice and your patients?
GB: I have maintained the regular flow of my clinical practice, but mostly through telephone calls. I only see patients in person if it’s an emergency and I need to do a physical exam.
As a doctor, you have to weigh the pros and cons of sending patients to the Emergency Department. If the risks of them getting sick and suffering complications, including death, from covid-19 are too high, you do everything you possibly can to keep them home. Since my patients are very vulnerable, we don’t know when we’ll be able to bring them back to the clinic, which is another source of anxiety for everyone. Ideally, I won’t bring anyone in until the authorities say it is safe for them to come to the Children’s.
What impact is the crisis having on families?
GB: Everybody is very concerned obviously. Thankfully, families are following all the government recommendations and staying home to avoid risks. As a mother of a child who is also vulnerable, I have a good idea of what it’s like and have much compassion for them.
Do you have any recommendations or tools for families?
GB: Please follow the authorities’ guidelines to the letter and reach out to the help lines if you are in distress. Please know that the teams at the Children’s meet regularly to align priorities and preparedness to remain mobile and flexible to ongoing needs. We are on this!
The majority of Dr. Bernard’s time (75 percent) is spent on researching leukodystrophies in her laboratory. She manages a team of ten people, comprised of research assistants and associates, as well as students. This is a difficult time for all of them, because most work at the MUHC Research Institute has been significantly reduced, in order to focus efforts on the crisis.
What is happening with your laboratory right now?
GB: We are lucky because several projects were on timelines that were wrapping up or put on hold without losing valuable data. One project – a new gene discovery – was completed and now we will be able to write it. Our projects on IPSC (induced pluripotent stem cells – which are used to make brain cells) was put on hold for now, but we are ready to restart at full capacity as soon as this crisis is behind us. Our mouse project had been slowed down significantly as per the MUHC-RI and McGill University recommendations, but we are confident that nothing will be lost and that we will be able to pursue our work where we left off after the Covid-19 pandemic.
What impact is this stoppage having from a productivity standpoint?
GB: I think it will slow us down, but this is the reality of living through a global pandemic. The priority is to follow the authorities’ instructions to save lives! So yes, I am worried about my lab’s productivity, but at the end of all this, I think granting agencies will make adjustments in the way they evaluate and fund projects. Since I have been a career researcher for almost 10yrs, I am established and experienced enough to sort it out well.
My team, who are all working from home, can continue to recruit patients and do questionnaires to collect data from them. We are also working on manuscripts and grant proposals remotely to reduce the impact of this on everyone’s productivity. I have an amazing team of superstars who are all helping each other out and making the best of the situation. I could not ask for anything better!
What will be your biggest challenges to overcome when this crisis is over?
GB: Getting back on track as fast as possible will be the biggest challenge. However, with my whole team supporting each other so harmoniously, we will succeed!
How can donors help?
GB: Extra funds will certainly help speed things up and get results, which we can then use as a lever to apply for grants. In research, you must work hard to get preliminary data, which is often donor funded. Donor funding is really what keeps us going.
What message would you like to send to donors?
Be safe, healthy and stay positive! Most importantly, a huge thank you for helping us make the lives of our patients better.
And thank you for your words of encouragement and gratitude, it means a lot and helps us go on with our work. Thank you everyone!
